.png)
In any one lifetime, there is a ceiling to the wisdom we can attain by our own accord. We are limited by the time we hold, and personal experiences and perspectives can only take us so far. But for a lot of our lives, we are shaped by the teachings of others. Others who have been where we want to be, others who have walked idiosyncratic paths, made mistakes, and learned hard-won lessons. Insight that we may not gain through our own revelations, but by soaking it up from the testimony of others. Something that we would call mentorship.
Something so simple: listening to another, spending time with another. It comes to shape a person, and if executed with precision and direction, it can come to change the world.
And so today, Surgical Data Science Collective (SDSC) is sharing some of the lessons that have coalesced from a hundred-year-old neurosurgery residency program – the program that helped shape our founder Dr. Daniel Donoho.
University of Southern California (USC)
The Department of Neurosurgery at USC is one of the oldest and most prestigious training programs in the US. For over a century, it has produced generations of renowned surgeons who continue to shape the landscape of neurosurgical care. This legacy – one that is deeply personal to Dr. Donoho – has blossomed from years of community building and mentorship from doctors that teach the next generation how to think, teach, and care. Chief among them being Dr. Gabriel Zada, Professor of Neurosurgery, Dr. Donoho’s personal mentor of 7 years, and now the current director of the Neurosurgery Residency Program at USC’s Keck School of Medicine.

Based out of LA General Medical Center, the USC residents have one of the country’s busiest hospitals and emergency rooms at their disposal. As one of the best operative training environments available, it leaves residents very adept in their surgical training, prowess, and clinical judgement. Dr. Zada has spent years helping prepare these residents for anything, and by investing in our future leaders, he too continues the cycle that has made this program what it is.
“It’s the best, it’s investing in the future. Amazing people go on to do even more amazing things than you can do.” – Dr. Zada
The Circle of Life
Dr. Zada is a quintessential example of how you can have both a busy and successful surgical practice, and a successful scientific career. He himself was shaped by several renowned members of the neurosurgical community, the first of whom was Dr. Edward Laws – one of the most prolific pituitary surgeons in history. He taught him to be uncompromising when it comes to patient outcomes:
“You must fight relentlessly for your patients and their families, and you must be a true disease expert. We are not just a pair of hands that can remove a tumor, we must also be well versed in every aspect of the disease.”
Another one of his mentors, and the reason he chose USC, was Dr. Martin Weiss. Dr. Weiss taught him to be the best doctor possible through the way that you take care of your patients. That “we don’t train technicians, we train doctors. We are responsible for the entire process.”
Spoken of at the highest level, these lessons run extremely deep within the network of USC’s alumni, and they will remain the foundation for generations to come.
Before “Surgical AI” Had Its Name
Long before artificial intelligence (AI) became a buzzword in healthcare, Dr. Donoho and Dr. Zada worked hand-in-hand to develop a cadaveric model that recreates a carotid artery injury – an adverse scenario in pituitary surgery that happens not infrequently. Once perfected, they used the model to train over 300 surgeons on managing the event, and in the process confirmed that the training improved both skill and performance.1 During this course, all the simulations were recorded, and after Dr. Donoho’s idea to track the instruments, they created one of the first open-access video datasets in pituitary surgery that could be used for machine learning applications.

Dr. Donoho really ran with it,” Dr. Zada recalls. “Because we had so many standardized videos, he could assess the frames and start doing the manual work that ultimately launched the computer vision parts of SDSC.”
This early work and methodology on kinematic and endoscopic skull base surgery cultivated the idea that if we can make surgery better understood, we can improve the quality and availability of surgical knowledge worldwide. This philosophy is at the core of everything SDSC is and does, and is a direct outcome of the great mentorship Dr. Donoho received during his residency. He realized that some of the most valuable surgical lessons are learned only by proximity, and began to ask: how do we get this to everyone?
The Lineage Continues
Years later, that same mentorship lineage led to a new opportunity within surgical AI.
When asked about AI in surgery, Dr. Zada said: “I’ve been skeptical about very little of it. Of course we have to be safe, but it’s like the internet, it’ll be the next revolution and you should harness it, not shun it or turn it away. We’re using it in a lot of different ways already, and I’m very excited about so many different things that it offers us. Even just for me as a researcher, it’s a huge tool.”
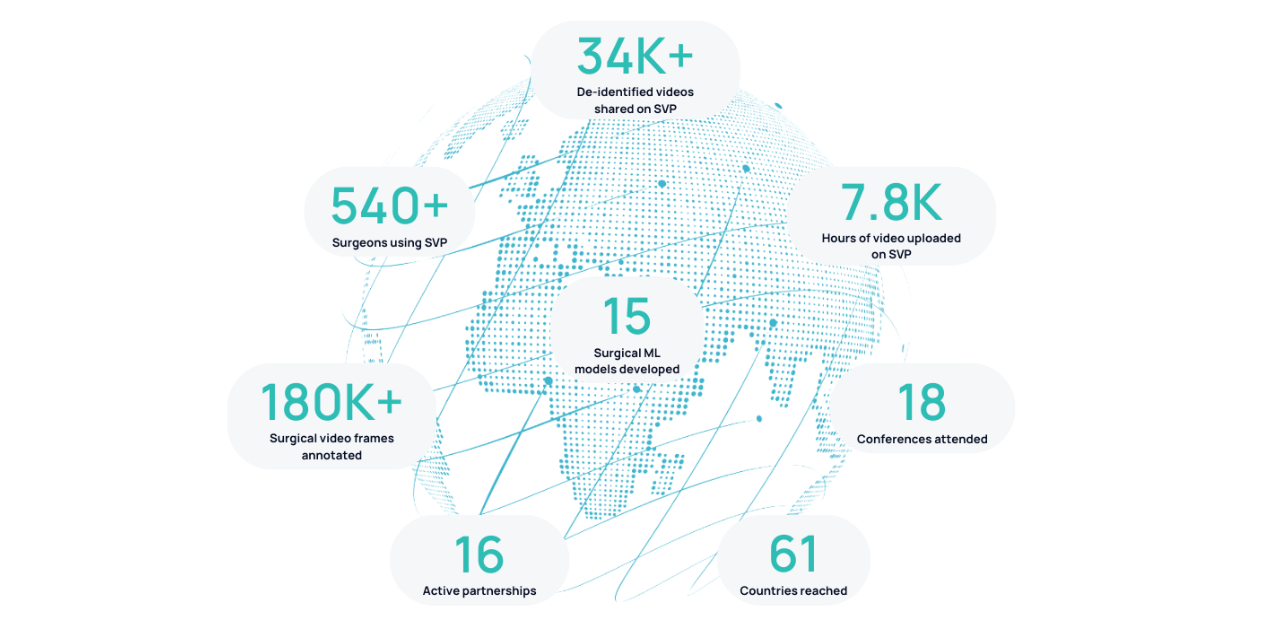
Years later, with SDSC a well-established organization, Dr. Donoho envisioned a research project that could target trainees even earlier in the cycle. And so, Danielle Levy became the first medical student to conduct and present independent research using real surgical videos on Surgical Video Platform (SVP).
Coming next: How medical student Danielle Levy became an early innovator in surgical data science, and what it means for the future of medical education.
1.Donoho DA, Pangal DJ, Kugener G, Rutkowski M, Micko A, Shahrestani S, et al. Improved surgeon performance following cadaveric simulation of internal carotid artery injury during endoscopic endonasal surgery: Training outcomes of a nationwide prospective educational intervention. Journal of Neurosurgery. 2021 Nov;135(5):1347–55. doi:10.3171/2020.9.jns202672



.png)
.png)