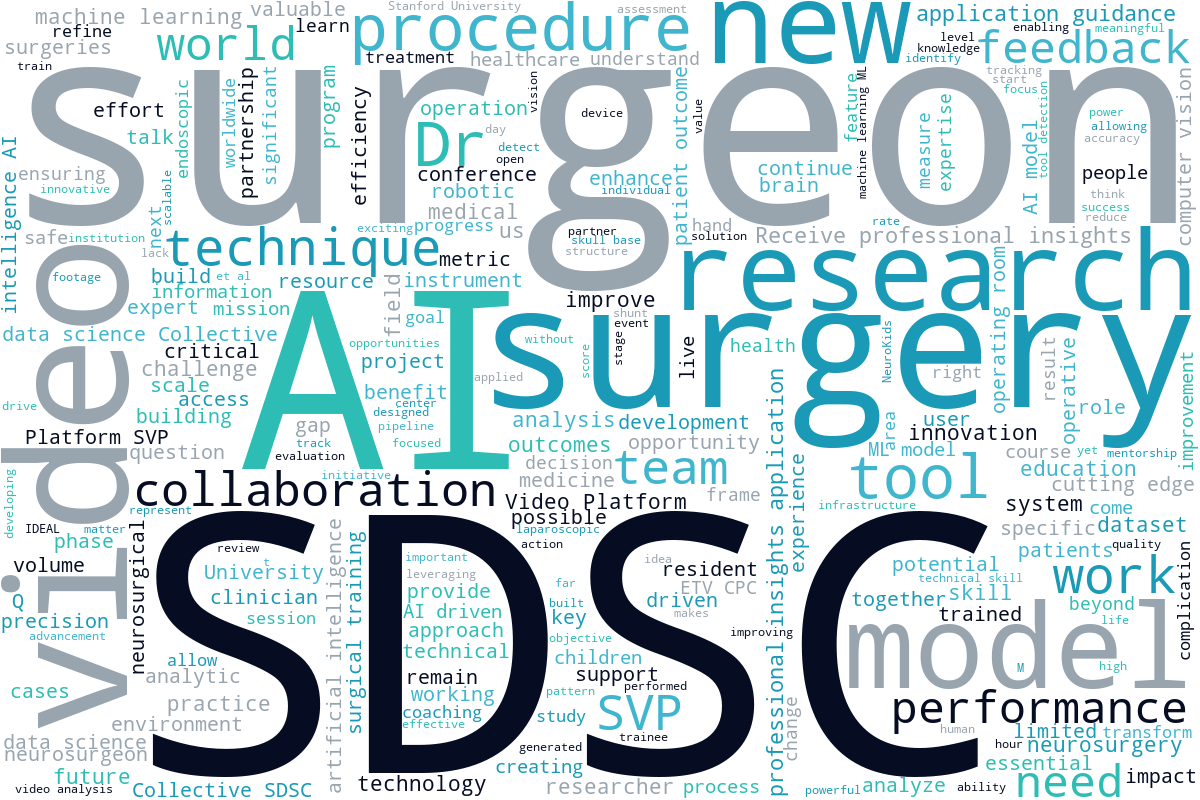
One of Surgical Data Science Collective’s (SDSC) crucial missions is to build on the lived experiences of surgeons. Before any work begins, we take the time to thoroughly understand the difficulties our researchers and clinicians are facing. That’s what makes our approach to artificial intelligence (AI) in surgery different.
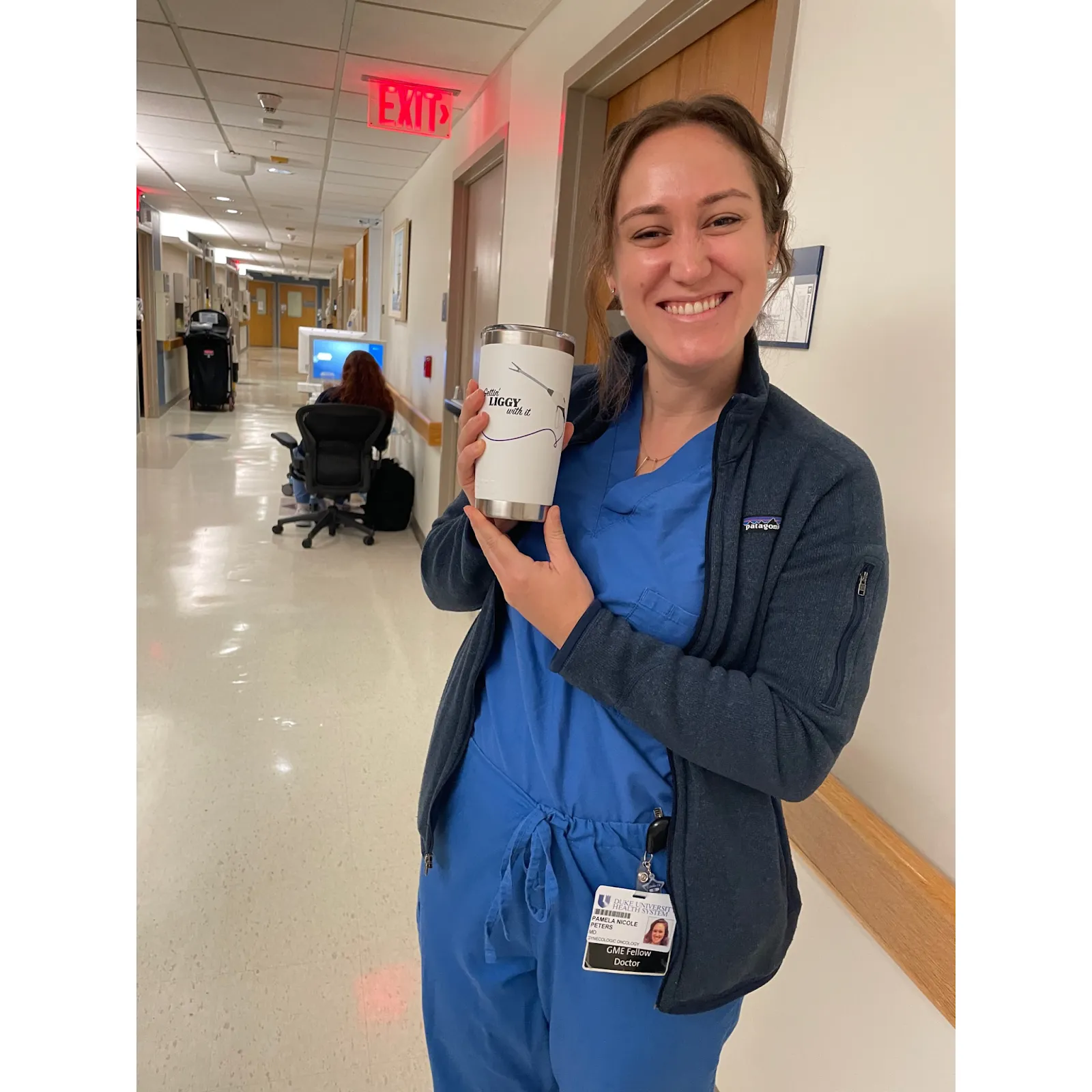
In our continuous effort to empower the OB/GYN community, we’re working closely with Dr. Pamela Peters, a gynecologic oncologist in Berkeley, California and clinical leader at SDSC, to understand how surgical video and AI can better serve practitioners at every stage of their career.
“Surgical training doesn’t stop at residency; it just gets lonelier.”
That’s how Dr. Peters describes the post-training gap in OB/GYN. Residents often rely on protocols or recorded cases before a procedure, but early-career surgeons are often left without feedback or mentorship once they’re practicing independently. They want to improve, but rarely have the time or tools to reflect critically on their own technique. Knowing how well you did it and how to get better would be of huge benefit, instead of just relying on what to do.
“The most obvious first application of computer vision technology is for residents,” Dr. Peters told us. “But it’s actually just as useful, maybe even more so, for early-career surgeons. After residency, you’re on your own.”
This is where SDSC can help.
Dr. Peters has been recording her cases for years – not just for documentation, but to revisit moments when she felt things could have gone smoother, and to identify opportunities for improvement. She wants to build a library of cases for trainees, but editing and organizing these videos takes hours. “In an era of AI, it seems like there has to be a better way.”

From Laparoscopy to Machine Learning: What AI Can Actually Do
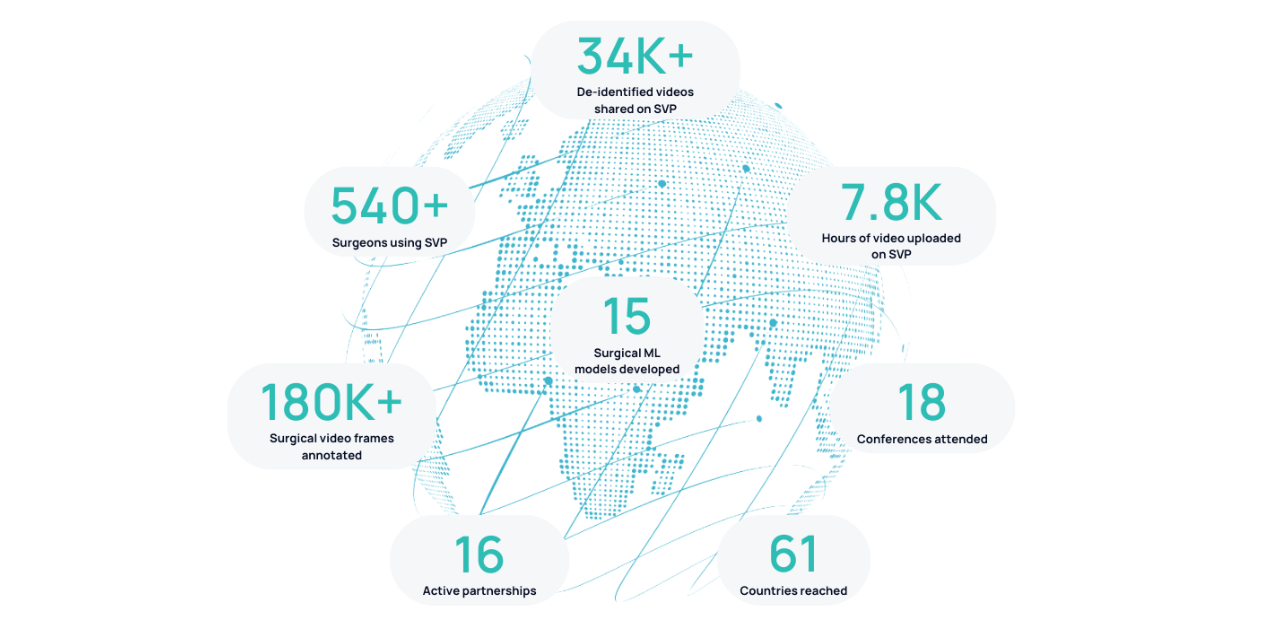
With SDSC’s Surgical Video Platform (SVP), that “better way” is starting to become real. Surgical video is a goldmine for education, but most of its value is locked behind hours of footage and a lack of tools for structured analysis. In OB/GYN, the opportunity is especially strong, as laparoscopic procedures produce exceptionally high-quality video. That clarity makes them ideal for computer vision analysis.
Our AI models can already detect tools and surgical phase transitions within surgical video. But what Dr. Peters and others are asking goes further: Can we measure surgical efficiency? Can we analyze tissue handling? Can we offer intraoperative guidance for identifying anatomical landmarks – like the ureter or key structures in the retroperitoneal space?
Dr. Peters compared it to the kind of performance feedback provided by the Athlete Intelligence feature on Strava: “What if we could make athlete intelligence for surgeons? It could feed back that you increased the speed of your vaginal cuff closure, but are lacking in efficiency elsewhere.” Right now, there’s no way to know that unless someone’s watching you – and often, no one is.
She also points to how much she’s come to value things like tension and exposure during surgery: “I’ve underestimated how helpful it is to have an assistant who knows how to pull tissue just right.” Like Dr. Ron Barbosa, she imagines a training model to recognize proper traction and countertraction – something that could radically improve learning for residents and refine technique for practicing surgeons.
What’s Next: A Call for OB/GYNs
We’re inviting more OB/GYNs to be a part of this. Whether you’re just starting out or have years of surgical experience, your videos and insight can help us build tools that truly serve the specialty. We’ve already started piloting this in simulated ectopic pregnancy surgery, and we’re looking for collaborators across general OB/GYN and minimally invasive surgery.
The challenges are real – uploading video is time-consuming, and integrating new tech into busy clinical workflows is hard. But we’ve built a system that works with surgeons and doesn’t add one more thing to manage. All you need to do is send us your videos and we’ll handle the rest.
We’ve seen this approach succeed in neurosurgery, where we’re collaborating with University College London (UCL) on pituitary tumor procedures. Now it’s time to bring it to OB/GYN.
If you’re recording your surgeries and wondering how to use them to improve training, share knowledge, or understand your own technique better – we want to hear from you. We’re especially interested in early adopters who want to shape the future of surgical video analysis in OB/GYN.
Let’s build this together.



.png)