.png)
The operating room is one of the most complex environments in medicine.
Constant analysis. Constant judgement. Constant interaction.
Every move, every decision, every success or setback could hold lessons for the next case. But we are letting huge amounts of this information slip through our fingers every day.
For Dr. Hani Marcus, neurosurgeon and Chair of the IDEAL Collaboration, changing that has become a defining mission.

Why Coaching is the IDEAL First Use Case for AI
In his clinical work, Dr. Marcus practices at one of the UK’s preeminent pituitary tumor surgery programs at the National Hospital in London. There, his team was the first in the world to introduce AI-assisted coaching for both pituitary surgery and the field of neurosurgery — a program that analyzes surgical videos to provide structured feedback for trainees and consultants alike.

This initiative has shown measurable benefits: higher-quality pituitary surgeries and fewer complications.1 It has also led to the collaboration between Surgical Data Science Collective (SDSC) and Dr. Marcus’ PhD student and senior resident, Dr. Danyal Khan, to deliver the Global Coaching Program.
Unlike real-time intraoperative AI, which carries high regulatory and ethical barriers, AI-assisted coaching operates offline and poses minimal risk to patients. It helps surgeons reflect on their performance and fosters open discussion.
Dr. Marcus has observed that AI can also act as a neutral facilitator in feedback sessions, easing cultural and hierarchical barriers:
“AI is quite useful to allow surgeons to share their practice in a safe way. It would be hard for a junior surgeon to say to a senior surgeon ‘you're not doing a great job here, this is how I would do it.’ The barrier culturally is too high. Whereas if the AI says to the senior surgeon ‘this is the metric which you didn't do so well’ it sometimes makes it easier for surgeons.” – Dr. Hani Marcus
Where Surgical Data Science Stands Today
Despite his success, Dr. Marcus is quick to point out that the biggest barriers to surgical data science are not technological. Recording and storing surgical videos, overcoming medico-legal concerns, and earning patient and surgeon trust remain major challenges.
“I’ve recorded every operation I’ve done since I was a trainee,” he says. “But most surgeons don’t record at all. In fact, many hospitals don’t even have the infrastructure to store videos.”
.png)
In robotic and laparoscopic surgery, where procedures are automatically recorded, surgical data science has flourished. For example, robotic prostatectomies and cholecystectomies have been generating vast datasets linking motion metrics to patient outcomes for years. Neurosurgery, however, has been slower to adopt these practices — partly due to technical and medico-legal challenges, and partly due to culture.
So, what are the barriers?
A few examples Dr. Marcus has encountered:
- Technical challenges of recordings: Many hospitals lack the bandwidth or storage for high-quality surgical video.
- Data medico-legal challenges: With complications being more impactful in the complex field of neurosurgery, individuals and institutions are becoming increasingly cautious about how their data is stored and shared. Bigger repercussions for high-stakes procedures = greater hesitation.
- Cultural adoption: Tradition can outweigh curiosity in surgical practice.
This is why SDSC plays such a vital role in the global surgical community.
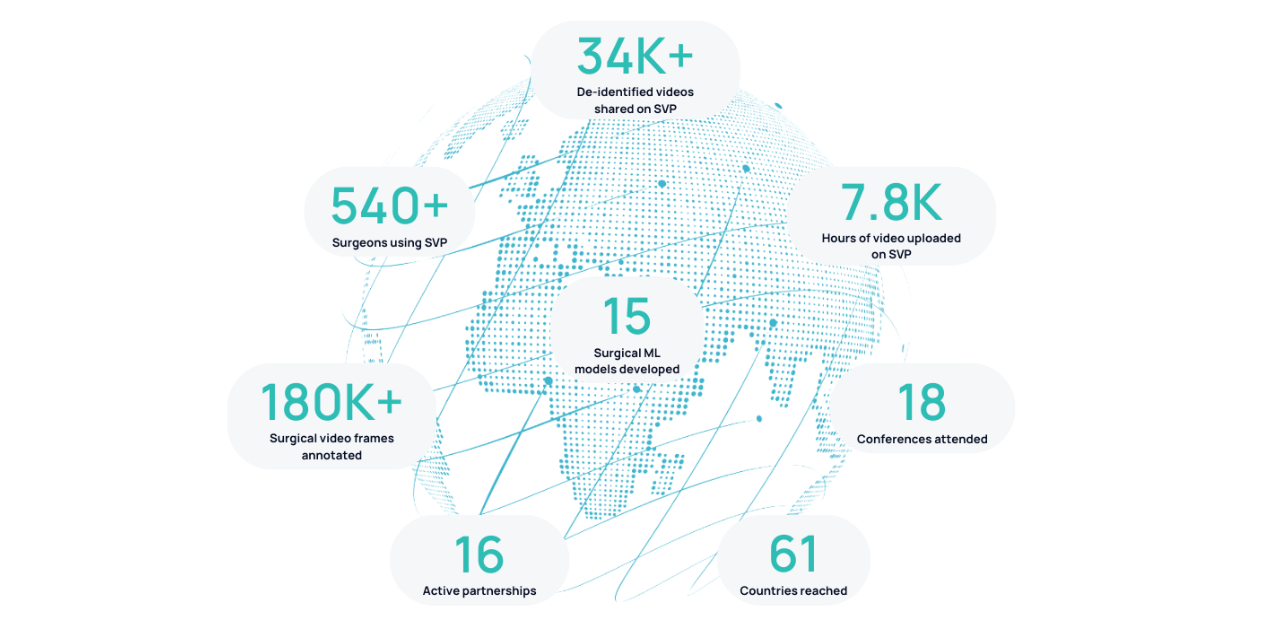
By building the infrastructure and a collaborative Surgical Video Platform (SVP) to collect, store, and analyze surgical video securely, SDSC helps bridge the gap between cutting-edge AI research and real-world clinical practice.
“The AI part is in many ways easy,” says Dr. Marcus. “The first difficulty is in providing infrastructure and allowing for data to be recorded and reviewed. Then if you have the option to share it with others, that makes collaboration much easier. That’s where SDSC has real value. It's a route for people to be able to upload data to even low- and middle-income countries and therefore use that to do coaching or anything else.”
By addressing these foundational barriers, SDSC aims to make surgical data science accessible, equitable, and scalable — enabling coaching, benchmarking, and ultimately better patient outcomes.
The Next Generation of Surgical Data Scientists
For those eager to contribute to this growing field, Dr. Marcus sees two equally valuable routes: come from medicine and learn engineering, or come from engineering and learn medicine. Either way, what matters is becoming “bilingual” enough to bridge the two worlds.
He sees surgical data science as an area of immense potential — one that will shape how surgeons learn, collaborate, and improve. “I’d advocate for surgical data science to anyone,” he says. “It’s going to be a huge part of our practice in the future. I’m excited to see where it goes next.”
Through leaders like Dr. Marcus, initiatives like IDEAL, and global collaborations like the Global Coaching Program, surgery is entering a new era. An era driven by data, guided by ethics, and powered by AI.
1. Khan DZ, Newall N, Koh CH, Das A, Aapan S, Layard Horsfall H, et al. Video-based performance analysis in pituitary surgery - part 2: Artificial Intelligence Assisted Surgical Coaching. World Neurosurgery. 2024 Oct;190. doi:10.1016/j.wneu.2024.07.219



.png)
.png)