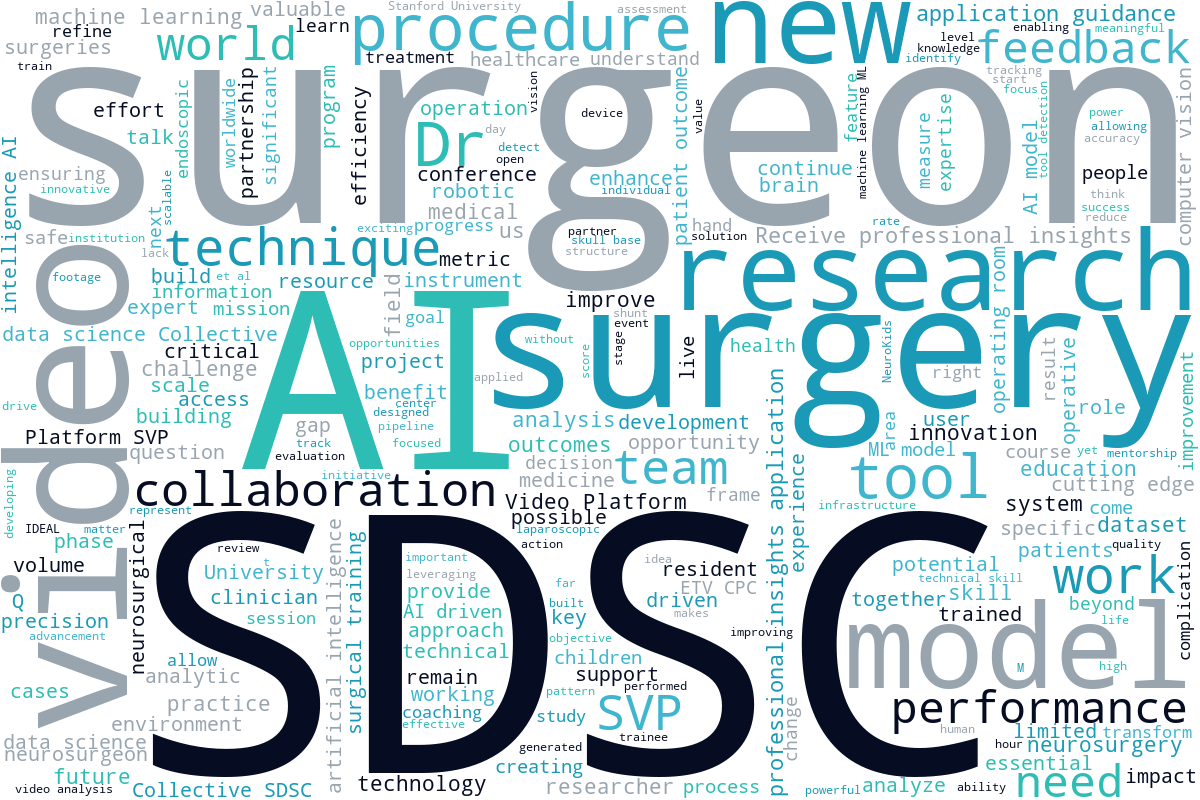
As 2025 draws to a close, we’d like to take a moment to reflect on the incredible community of surgeons we have built in 2025. This year, we’ve had countless conversations with surgeons across disciplines – OB/GYN, neurosurgery, trauma, surgical oncology – with so many converging on shared ideas about artificial intelligence (AI) and its place in the surgical data science realm.
But to whittle it down to a singular core truth: surgical excellence is hard to measure, hard to teach, and even harder to improve without data.
Our community is clamoring for so many of the same things, regardless of specialty:
- Better tools for reflection and feedback
- Ways to overcome the educational loss derived from shrinking case volume
- Infrastructure to record and learn from surgical video
- Transparent, evidence-based methods to measure skill
- A culture where sharing surgical video isn’t intimidating.
This list is by no means exhaustive, but it’s just about enough to highlight how important the implications of surgical data science are to this community. They’re calling for help solving problems that can’t be fixed inside any one hospital, department, or specialty, and that’s one of the very reasons why SDSC exists.
1: Case Volume
Across every specialty we spoke to, declining case volume emerged as one of the most pressing issues.
OB/GYN: There aren’t enough teaching cases to develop mastery
Dr. Pamela Peters described the typical educational pathway in the OB/GYN field that provides a foundation for gynecologic surgery, but not enough to master it.
“Residency gave me the basics, but not the confidence or the case volume.”
“There’s little national effort to address declining surgical volume in gynecology, so this is something we can do more about.”
And in gynecology where the average surgeon performs fewer than nine hysterectomies – an extremely relevant surgery – per year, confidence and independence become that much harder to achieve.1

This is even more relevant for patients. Low operative volumes are associated with high case-fatality rates from common, treatable surgical conditions.2 And considering that each year an estimated 50 million adults have at least one postoperative complication, 3.5 million of whom die within 30 days of surgery every year, an expansion of surgical volume is crucial to ensuring that each patient receives the best possible outcomes following their surgery.3
Neurosurgery: More fellowships, less autonomy
Neurosurgeon Dr. Jacob Young told us that residents increasingly pursue additional fellowships – not just for sub-specialization, but because case numbers are declining and autonomy is shrinking.
“Anything that can optimize the educational value of each case has the potential to get trainees ready for independent practice faster.”
SDSC’s take:
As surgeons struggle to receive the optimal number of hours in the OR, they’re asking for ways to extract more learning from every case. This is exactly what objective video feedback and automated performance metrics can provide.
2: The Post-Training Gap
We have repeatedly heard from early-career surgeons that learning shouldn’t end when official training does.
Dr. Peters stated it clearly: “After residency, you’re on your own.”
Dr. Young echoed it: “There isn’t a lot of opportunity to continue as a learner outside of formal courses.”
Even with access to senior colleagues in world-renowned institutions, seeking mentorship can become opportunistic and unfruitful.
SDSC’s take:
This loneliness derived from an absence of structured feedback post-training is one of the strongest needs the Surgical Video Platform (SVP) can address.
Surgeons want something like Strava’s “Athlete Intelligence” for their own surgical performance. A place where they could upload videos to identify the trends, patterns, and strengths in their work. Or potentially a monthly report that helps track progress and keep learning consistent.
3: AI for Coaching
Another dominant cross-disciplinary message was the idea that AI holds immense coaching potential, and is a facilitator of honest conversation among clinicians.
Neurosurgeon Dr. Hani Marcus emphasized that AI’s value is in its ability to soften the professional hierarchy’s impact on learning.
“AI can say things that a junior surgeon can’t. If an AI points out a metric, it becomes easier for surgeons to discuss their practice.”
AI acts as a neutral observer, and therefore a catalyst for real feedback.
SDSC’s take:
Coaching is offline, low-risk, universally beneficial, and not dependent on perfect AI. It is an easy first use-case that we can deliver at scale. Our Global Coaching Program is quintessential of this.
4: Infrastructure: The Unseen Barriers to Everything
If we had to pin down just one essential lesson from the entirety of 2025, it’s this one:
The single biggest barrier in surgical data science is infrastructure.
“The difficulty is in providing infrastructure and allowing for data to be recorded and reviewed. Then if you have the option to share it, that makes collaboration much easier.” – Dr. Hani Marcus
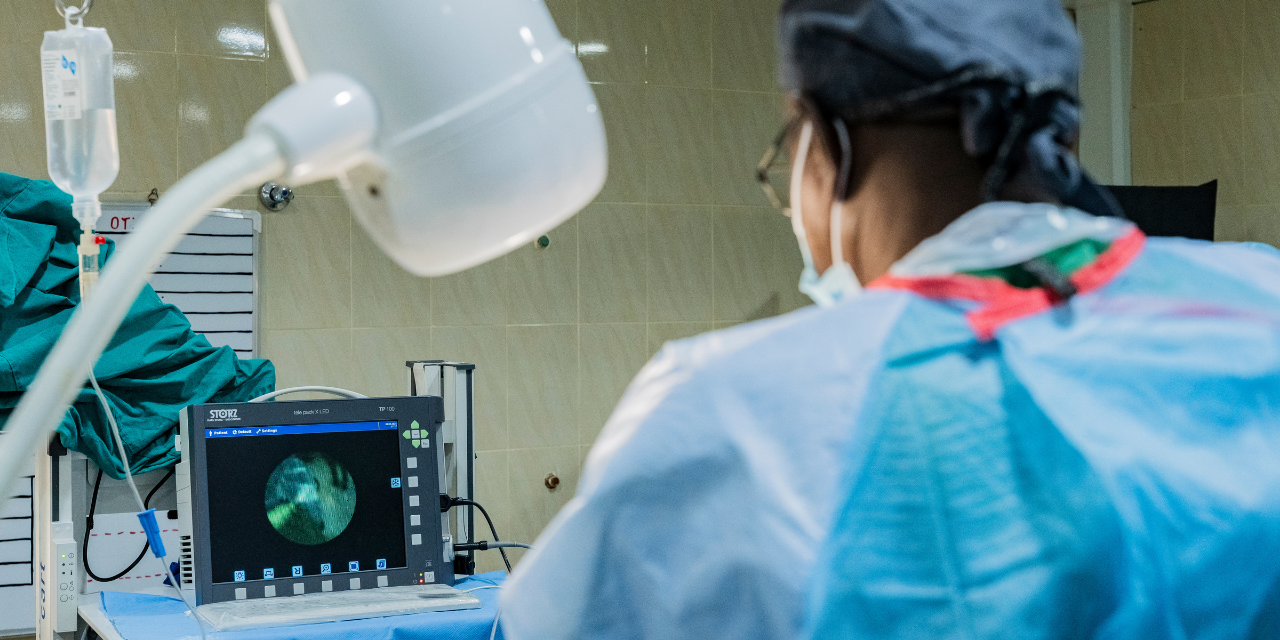
Across hospitals, many surgeons don’t record video at all, fewer have sufficient storage, fewer still can upload securely, and very little have institutional support to make it easier. Even major centers of excellence struggle with bandwidth limitations, storage costs, lack of recording defaults, and so many other medico-legal anxieties.
SDSC’s take:
Our non-profit mission resonates so strongly because surgeons want someone to build the foundational layer, and they need it to be built by an organization they can trust. Every day our talented teams are curating the infrastructure that allows:
- Video capture
- Storage
- Secure sharing
- Global collaboration
- AI-driven feedback
- Research and mentorship across borders
This is the layer that commercial companies don’t build. This isn’t for profit, it’s for patients.
5: Skill Visibility
A hot topic that almost all of our Data Science Roundtables cover. Across specialties, surgeons expressed enthusiasm about a future where surgical skill is measurable, not anecdotal. To do this, they need a better system.
SDSC’s take:
The evidence is right in front of us, and it confidently shows the future is in quantifying technical proficiency. But this is not a small feat, and SDSC works hard every day to scale this impact globally.
Our 2026 Aspirations + A Short Message From Dr. Daniel Donoho
Surgeons are telling us:
“We need infrastructure.”
“We need feedback.”
“We need coaching.”
“We need ways to learn when case volume falls.”
“We need a safe, neutral way to talk about performance.”
“We could do so much with our surgical video, if only we had the tools.”
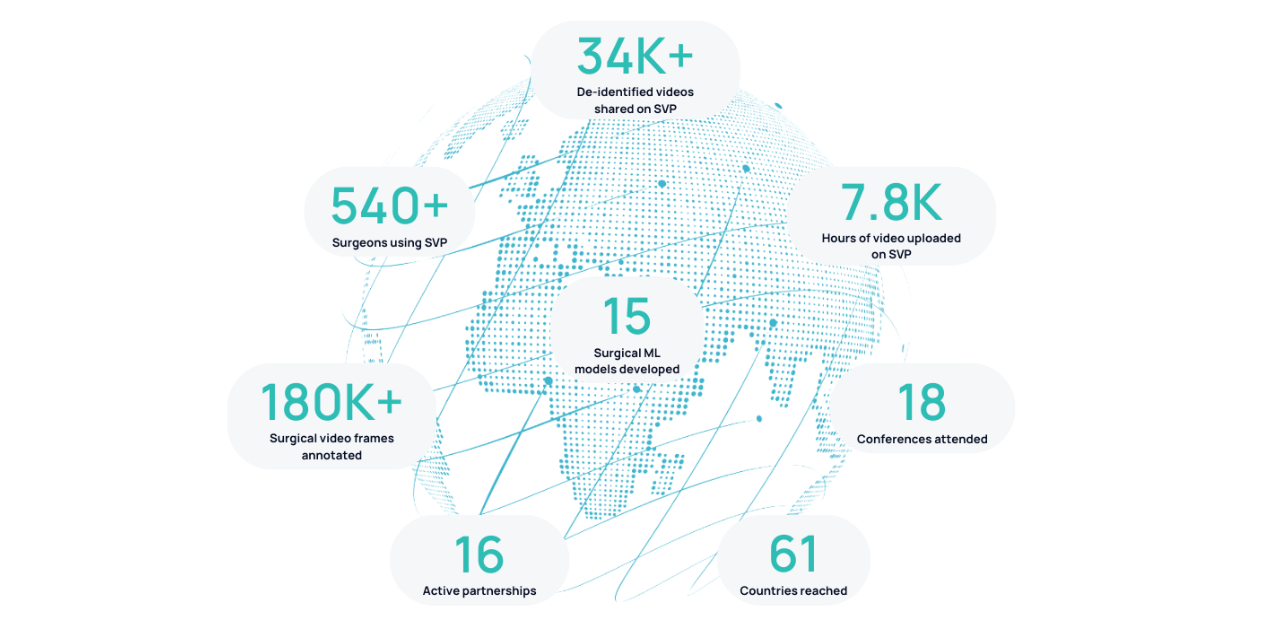
The Surgical Video Platform (SVP) is the key to unlocking all of this potential, and we want to empower as many surgeons as we can, no matter where you are in the world.
We can’t do it alone, and we are grateful to every one of our wonderful collaborators who have participated in so many of these important conversations across the year. We are listening, and we are building with you, for you.

A few words from our founder Dr. Daniel Donoho:
“2025 has been a pivotal year that we needed as an organization across every single aspect. 2026 will be the impact year that it needs to be because of the really monumental and impressive work that everyone has put in over 2025 to make SDSC poised for impact in the real world. We have never looked stronger, and I am confident that we will succeed.”
1. Ewies AA. Obstetrics and gynaecology: One specialty or two? Journal of Obstetrics and Gynaecology. 2023 Jul 4;43(2). doi:10.1080/01443615.2023.2227031
2. Meara JG, Leather AJ, Hagander L, Alkire BC, Alonso N, Ameh EA, et al. Global surgery 2030: Evidence and solutions for achieving health, Welfare, and Economic Development. The Lancet. 2015 Aug;386(9993):569–624. doi:10.1016/s0140-6736(15)60160-x
3. Nepogodiev D, Picciochi M, Ademuyiwa A, Adisa A, Agbeko AE, Aguilera M-L, et al. Surgical health policy 2025–35: Strengthening Essential Services for tomorrow’s needs. The Lancet. 2025 Aug;406(10505):860–80. doi:10.1016/s0140-6736(25)00985-7



.png)
.png)