.webp)
For over a century, the combined field of obstetrics and gynecology (OB/GYN) has delivered an all-in-one approach to the care of women’s health. Introduced in the 1920s, this dual training pathway was designed to ensure comprehensive care, but with the evolution of gynecologic surgery, the lines between the two specialties have grown more distinct.
In a 2014 journal article, OB/GYN Dr. Javier Magrina argued that the only commonality between obstetrics and gynecology may simply be its patient population, rather than procedural foundations.1 And in an era of increasingly specialized medicine, many are beginning to ask: is it time for OB and GYN to stand separately?
We sat down with Dr. Pamela Peters, a gynecologic oncologist and the clinical lead for OB/GYN research at Surgical Data Science Collective (SDSC), to discuss how surgical training in gynecology has changed, what’s at stake for patients and trainees, and how we can work together to bring about better solutions.
“Residency is only the very beginning of building confidence.”
Dr. Peters trained in the current era of minimally invasive gynecologic surgery (MIGS). But even with that foundation, she knew she needed more. Following residency, she completed an additional three years of surgical fellowship.
.webp)
“Residency gave me the basics, but not the confidence or the case volume,” she says. “It provides the foundation of surgical training, but typically doesn’t provide the gynaecology case volume to be highly competent immediately after training.”
She’s not alone. Surgical case volume in gynecology has been dropping for decades. In the United States, the number of hysterectomies performed fell by 20% between 1980 and 2007, while the number of gynecologists rose by 57%2. That means the average gynecologist today performs fewer than nine hysterectomies per year – down from 28 in the 1980s.2
Less surgical exposure means less confidence at graduation. One study comparing OB/GYN residents with those who completed an additional fellowship year of laparoscopic training found that none of the fourth-year residents could perform basic suturing tasks correctly, while every fellow could – faster and with fewer errors.3
That is not a critique of OB/GYN residents. It’s a reflection of a system that is trying to do too much, for too many, with too few resources.
Time to Split the Tracks?
Dr. Peters is a strong proponent of separating the OB and GYN training tracks.
“It just makes sense,” she says. “You need surgical skills for OB, absolutely – for caesareans, vaginal repairs, managing complications. But gynecologic surgery is a whole other world. Vaginal procedures, hysterectomies, laparoscopic and robotic skills – it’s a different skill set.”
Separating the tracks would allow for deeper focus, better training, and ultimately, better patient outcomes. It could also help relieve some of the pressure residents feel – especially in a field that is both female-dominated and, ironically, burdened by expectations to “do it all”.
“There’s a gendered dynamic here,” Dr. Peters notes. “This is a specialty that treats women, is largely staffed by women, and yet we’re here asking trainees to be everything: obstetricians, surgeons, primary care doctors, and often researchers. It’s a setup for burnout. Women’s health deserves the same focused, specialized care as any other field.”
And burnout is indeed rising. A 2019 Medscape survey of 15,000 doctors in the U.S. found that gynecologists ranked amongst the most burned-out specialists in medicine.4

A Call for Creative Solutions
Despite her specialization in gynecologic oncology, Dr. Peters sees more benign gynecologic cases referred to her than ever before – cases that would previously have been routine for generalists. This shift is a direct consequence of a system-wide trend towards low-volume surgical practices.
It’s not an easy problem to fix. But it’s not one we can ignore.
“There’s little concerted national effort to address the declining surgical volume in gynecology,” she says. “So this is something we can do more about.”
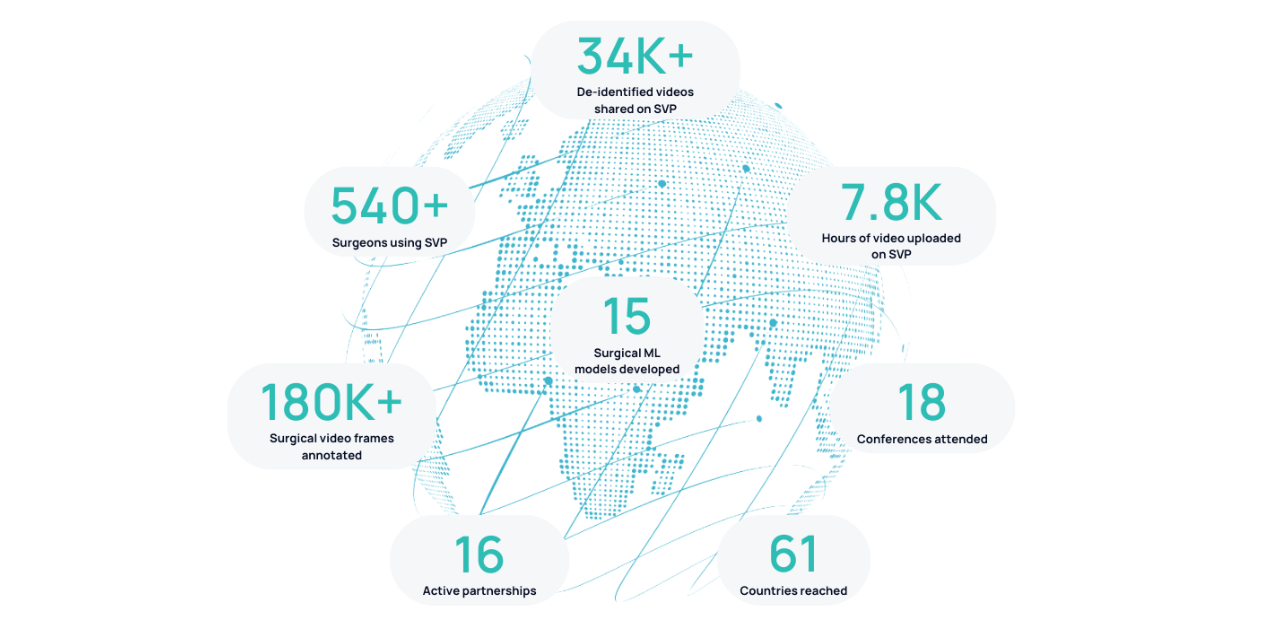
We can’t change the trend of declining surgical volume, but SDSC is committed to supporting surgical education and improving patient outcomes through data, research, and collaboration. MIGS is an ideal specialty to benefit from AI and surgical video-based research: procedures are performed with endoscopic video cameras, so recordings are plentiful. Practitioners immediately understand the pedagogical benefit of seeing many more cases than they would see by themselves, and AI analysis can lead to accelerated learning, expertise development, and groundbreaking research. By working hand-in-hand with clinicians, educators, and trainees, we can rebuild confidence, redefine excellence, and reshape what’s possible in OB/GYN training.
The solution isn’t to ask less of our residents. It’s to give them more of what they need to succeed.
Want to learn more about how SDSC is supporting surgical training and research in OB/GYN and beyond? Contact us or join our community to get involved.
- Magrina JF. Isn’t it time to separate the O from the G? Journal of Minimally Invasive Gynecology. 2014 Jul;21(4):501–3. doi:10.1016/j.jmig.2014.01.022
- Ewies AA. Obstetrics and gynaecology: One specialty or two? Journal of Obstetrics and Gynaecology. 2023 Jul 4;43(2). doi:10.1080/01443615.2023.2227031
- Akl MN, Giles DL, Long JB, Magrina JF, Kho RM. The efficacy of viewing an educational video as a method for the acquisition of basic laparoscopic suturing skills. Journal of Minimally Invasive Gynecology. 2008 Jul;15(4):410–3. doi:10.1016/j.jmig.2008.03.012
- Medscape National Physician Burnout, depression & suicide report 2019 [Internet]. [cited 2025 Jul 25]. Available from: https://www.medscape.com/slideshow/2019-lifestyle-burnout-depression-6011056?faf=1#3



.png)
.png)