In Part 1, we explored a fundamental truth that has been hiding in plain sight: technical skill is a powerful determinant of surgical outcomes. And now that we understand just how much proficiency matters, we can begin to ask the inevitable, but more complicated question:
How do we scale this impact to every surgeon, hospital, and patient in the world?
Modern artificial intelligence (AI) is giving us a way forward. And the implications, especially in the places where safe surgery is needed most, could be life-changing.
Why This Matters Even More in Low-Resource Settings
The stakes of surgical performance are universal, but their consequences are not.
The burden of postoperative mortality disproportionately falls on patients in low- and middle-income countries (LMICs).1 A complication that might be regrettable in a high-resource hospital, for example an infection, cerebrospinal fluid (CSF) leak, or need for re-operation, can be disastrous in underserved settings. Re-operations may be unavailable, post-operative infections may go untreated, and small technical variations can determine whether a patient makes a full recovery, or is left to suffer the burden of preventable disability.
Improving the way surgery is performed carries enormous importance for global health.
An example of this is Surgical Data Science Collective’s (SDSC) work on endoscopic third ventriculostomy with choroid plexus cauterization (ETV-CPC) – a procedure developed by NeuroKids founder Dr. Benjamin Warf to relieve hydrocephalus in infants and adults. This disease perfectly demonstrates how technical differences can make such a profound impact on outcomes, as the ETV-CPC procedure is extraordinarily sensitive to technique, and small variations in CPC can dramatically alter success rates.2
As SDSC’s founder Dr. Daniel Donoho noted in our recent blog, SDSC is helping test a new methodology for training surgeons to perform ETV-CPC with the goal of
“increasing the number of trained surgeons and therefore the number of surgeries performed each year for children with hydrocephalus around the world – ultimately reducing death from neurologic disease and disability.”

When resources are limited, preventing complications through improved technique is far more impactful than treating them afterward. When complications can’t be treated, skill becomes the treatment.
From Guesswork to Quantification
Surgical education has relied on an apprenticeship-style model of training for decades. And with the arrival of surgical data science, we can go on to do something extraordinary:
Turn performance into measurable, analyzable data.
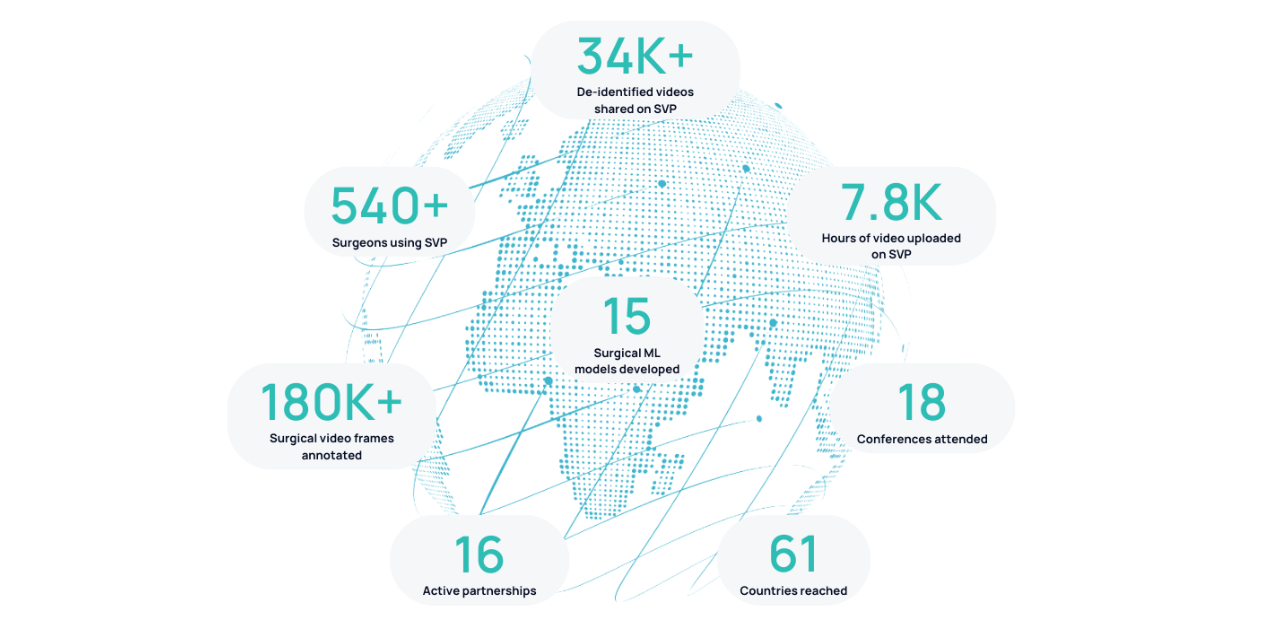
SDSC’s Surgical Video Platform (SVP) is the first step in this transformation. It allows surgeons and researchers to upload, annotate, and analyze surgical video at scale, using AI designed specifically for operative data.
Plus, our machine learning (ML) models always begin with an extra head start thanks to our academic collaborator Dr. X.Y. Han. With the help of his computational resources at the University of Chicago, we are able to co-develop models that are already familiar with complex surgical environments. From there, we can analyze:
- Tool usage patterns e.g. use frequency, spatial tracking, area covered, speed, accuracy, tool timeline
- Temporal flow of an operation
- Procedural phase breakdown

These metrics are some of the first stepping stones to answering an extremely important question: How did technical performance influence what happened to the patient?
We can only begin to make a dent once the right tools are in the right place. And so the ML team at SDSC is working tirelessly to keep SVP at the cutting-edge of this technological breakthrough.
Responsibly Bringing AI Into Surgical Practice
AI will never replace surgical judgement – and it shouldn’t!
As Stanford neurosurgery resident Dr. Dhiraj Pangal put it:
“The insights don’t come from the model. The model produces the data we use to derive the insights. The meaning comes from humans and experts who design the analysis.”
Imagine if all residency programs used objective video metrics to accelerate learning curves, as discussed by Dr. Sem Hardon in our Data Science Roundtable Series. Imagine researchers asking global-scale questions about technique variation, performance, and outcomes – using data, not anecdotes.
The future is already emerging:
- Dr. Sandeep Nayak – also a strong believer that AI is only ever as good as the human it teams up with – is using SVP to standardize his RABIT technique. By identifying which micro-steps correlate with the best patient outcomes, he is using these insights to make the procedure adoptable on a more global scale.
- Neurosurgeons at Muhimbili Orthopaedic Institute (MOI) in Dar es Salaam, Tanzania are using SVP to fight resource constraints and ensure a global standard of neurosurgical care for their patients.
- Dr. Jacob Young is breaking the “no feedback is good feedback” culture by using objective data that could change the way residents progress in microsurgery.
- University College London’s (UCL) Global Coaching Program is using SVP and AI-assisted feedback to scale expert coaching worldwide.
- Dr. Hani Marcus, guided by the IDEAL framework, is pioneering ways to integrate computer vision responsibly into routine surgical practice.
The community is also expanding into the OB/GYN field, where surgeons such as Dr. Pamela Peters are guiding our break into maternal health. She speaks openly about how AI can help rebuild confidence, improve learning opportunities, and gain objective feedback previously unavailable in the field.
These leaders are proving that when performance becomes measurable, coaching becomes scalable, outcomes become improvable.
Measuring What Matters
The conclusion is clear:
Surgical skill drastically impacts patient outcomes.
Now the technology to measure it exists, and the responsibility to use it belongs to all of us. By combining surgical expertise with data science, we can finally transform technical skill from a hidden variable into a measurable driver of improvement.
SDSC is building the tools to make this shift possible, and our global community of clinicians, educators, and scientists is already shaping what this future will look like, because:
Once you can measure skill, you can improve it.
Our patients need us, and this is a giant step towards equity for them all.
1. Nepogodiev D, Picciochi M, Ademuyiwa A, Adisa A, Agbeko AE, Aguilera M-L, et al. Surgical health policy 2025–35: Strengthening Essential Services for tomorrow’s needs. The Lancet. 2025 Aug;406(10505):860–80. doi:10.1016/s0140-6736(25)00985-7
2. Fallah A, Weil AG, Juraschka K, Ibrahim GM, Wang AC, Crevier L, et al. The importance of extent of choroid plexus cauterization in addition to endoscopic third ventriculostomy for infantile hydrocephalus: A retrospective North American observational study using propensity score–adjusted analysis. Journal of Neurosurgery: Pediatrics. 2017 Dec;20(6):503–10. doi:10.3171/2017.7.peds16379



.png)
.png)