The Hidden Emergency in Children’s Brains
Hydrocephalus is one of the most common and devastating neurological conditions affecting infants and children worldwide. Caused by a buildup of cerebrospinal fluid (CSF) – fluid that surrounds and protects the brain and spinal cord – in the brain, hydrocephalus results in dangerous intracranial pressure, head-enlargement, and severe disability or death if left untreated.
.webp)
For decades, hydrocephalus was primarily treated with a shunt – a small tube that drains excess fluid from the brain to the abdomen. Shunts are lifesaving, but they can also fail catastrophically. They degrade, they migrate, they clog, and a sudden halt in function can leave families in rural or resource-limited areas in desperate situations. Shunt failure is a serious emergency, yet reaching a neurosurgeon in time is often impossible.
A Better Blueprint for Hydrocephalus Surgery
Recognizing this challenge, Dr. Benjamin Warf, founder and chairman of NeuroKids, pioneered a new technique in Uganda: combining endoscopic third ventriculostomy (ETV) with choroid plexus cauterization (CPC). This dual procedure opens up a new pathway for CSF to flow out of the brain, and also reduces CSF accumulation by burning off areas of the choroid plexus (CP) – part of the brain responsible for producing CSF. Together, ETV/CPC offers a way to liberate children from a lifetime of shunt dependence.
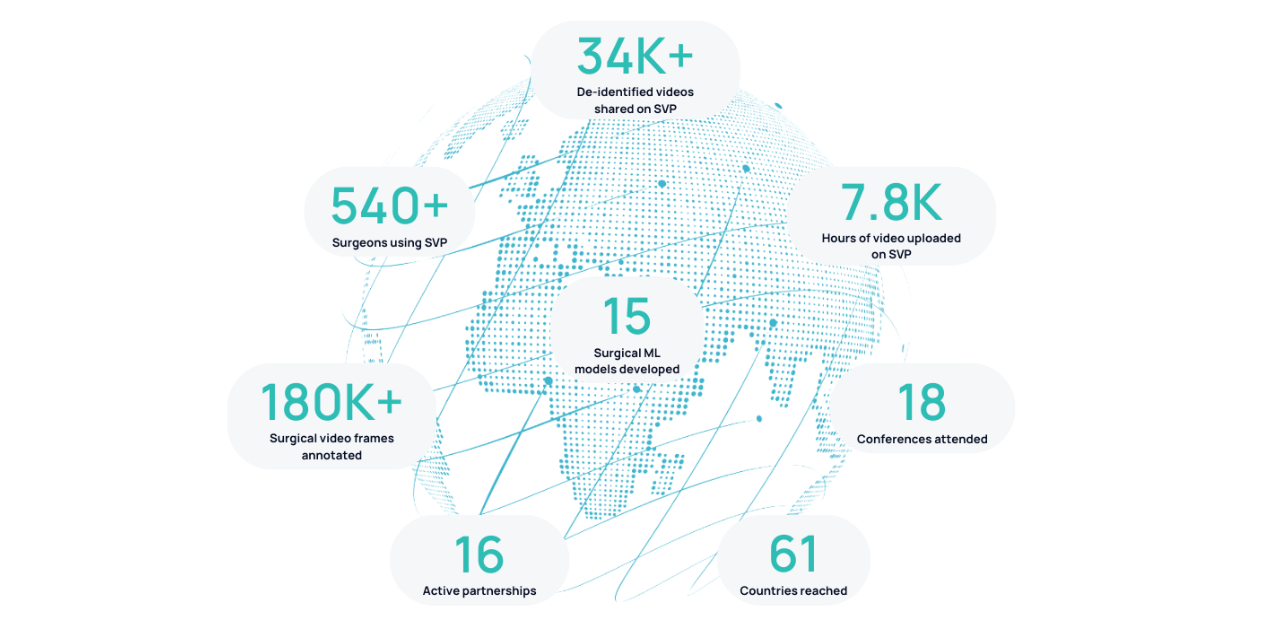
Since then, more than 10,000 ETV/CPC procedures have been performed, and NeuroKids has trained surgeons across Africa, Asia, and the US. But the traditional apprenticeship model of surgical training – one expert teaching one trainee in one hospital – simply cannot keep up with the demand. Hundreds of thousands of children need this surgery each year, and the global community needs scalable training and evaluation tools.
Are we cauterizing enough?
Partnered with NeuroKids, Surgical Data Science Collective (SDSC) is using surgical video and artificial intelligence (AI) to help tackle this immense problem. But first, a major surgical challenge still remains: how much of the CP needs to be cauterized? Surgeons know that cauterizing more CP reduces the chance of needing a shunt, but there’s still uncertainty around where to cauterize, how much, and whether certain hard-to-reach regions make a meaningful difference.1
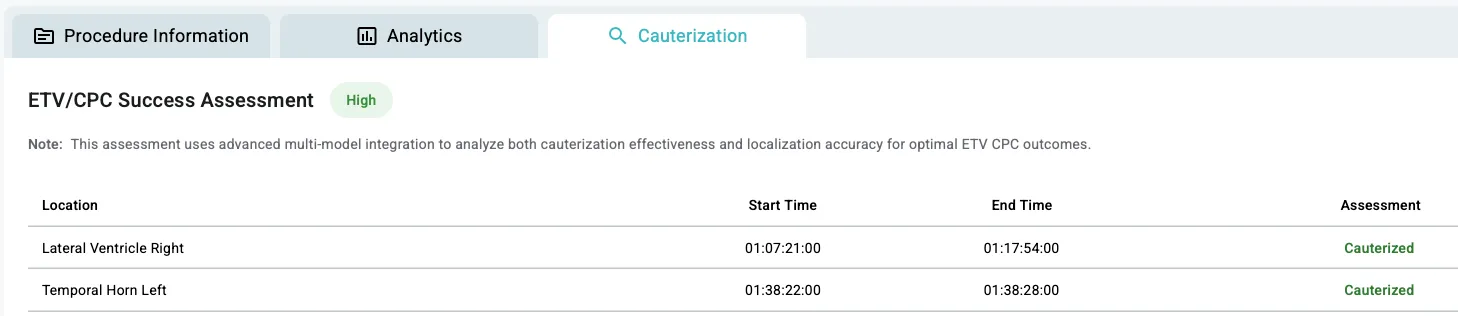
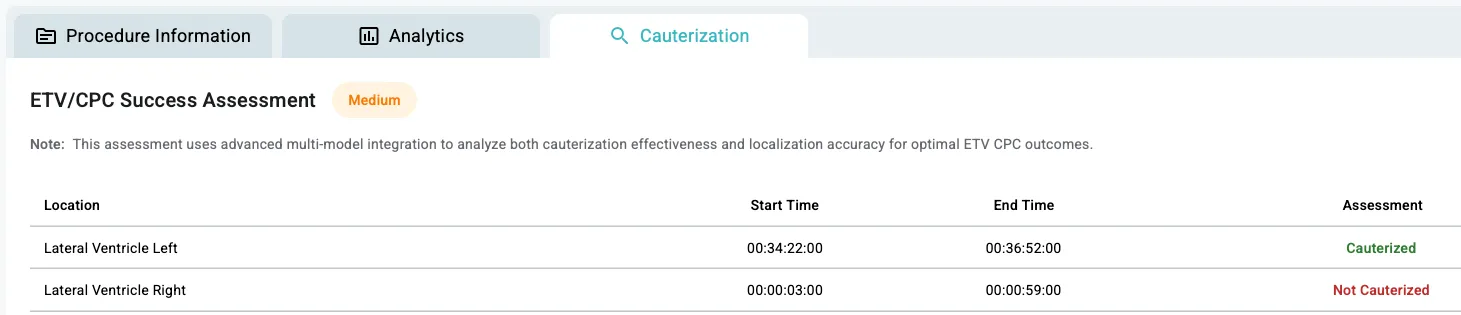
With the help of SDSC machine learning (ML) engineers Jack Cook and Kaan Duman, Surgical Video Platform (SVP) can now analyze ETV/CPC surgeries, helping surgeons understand both what they did and how well they did it. This ML model runs directly on the Surgical Video Platform (SVP) and is available to any user who uploads ETV/CPC case videos.
It utilizes a ResNet/ViT+MSTCN++ deep learning architecture with two parallel models and an integration logic:
- Localization model (Resnet50+MSTCN++ developed by Kaan) – Detects which region of the CP the surgeon is operating on:
- Left lateral ventricle
- Right lateral ventricle
- Left temporal horn
- Right temporal horn
- Cauterization model (ViT+MSTCN++ developed by Jack) – Detects whether the surgeon is actively burning CP tissue and distinguishes between cauterization of the CP versus other tissue.
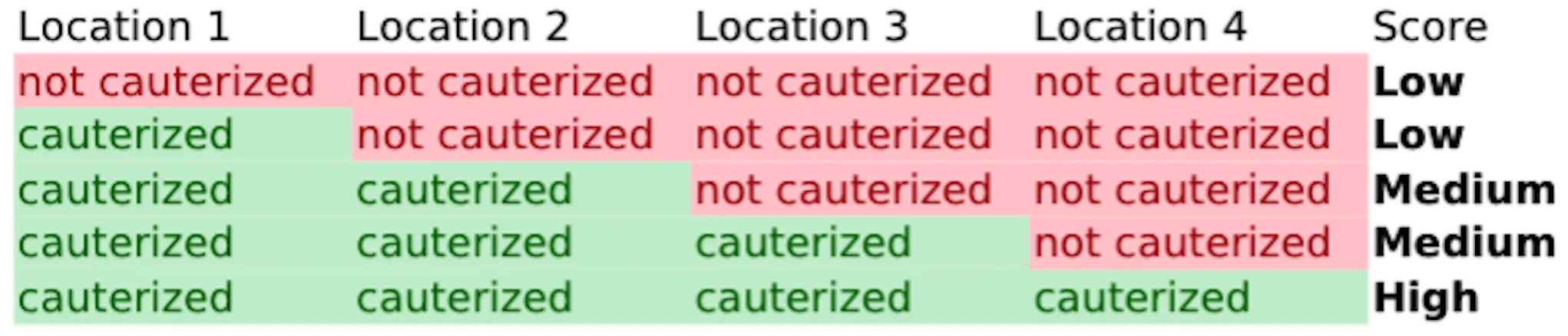
- The model outputs are combined: did cauterization occur, and was it adequately performed across the four regions? The platform then provides a simple score – high, medium, or low – which transforms hours of blurry, liquid-filled video into actionable insights that experts alone would struggle to capture.

From Blurry Videos to Clear Answers
Surgeons currently record whether they performed CPC using crude checkboxes: yes or no. This is massively subjective, time-consuming, and frequently inaccurate. With SDSC’s model, surgeons can upload their videos and immediately receive structured, objective analysis of how much choroid plexus was cauterized and where.
Along with accelerating feedback and learnings from past cases, this initiative is creating a foundation for global outcome research. Over time, the linking of surgical technique to patient outcomes can help the hydrocephalus community answer critical questions like:
- Does cauterizing more CP really reduce the chance of needing a shunt later?
- Is reaching difficult areas like the temporal horns worth the added risk?
- What level of cauterization coverage leads to the best outcomes?
Beyond hydrocephalus, this is about creating a new way to train surgeons and decipher important surgical nuances on a global scale – a digital first-approach that supplements traditional mentorship with data-driven insights. ETV/CPC may be the first domino to fall, but the same methodology can be extended to treating spina bifida, epilepsy, brain tumors, and beyond.
As Dr. Daniel Donoho, SDSC’s founder, explains:
“We’re opening up a new frontier of knowledge and practice. This is disruptive work – imperfect by definition – but it’s something no one has ever attempted at scale. We’re not just iterating; we’re changing how surgery is taught, evaluated, and understood.”
A Partnership to Change the World
NeuroKids is now working across 18 sites in 14 countries and SVP is supporting them every step of the way. Already, over 200 ETV/CPC procedures have been uploaded and analyzed, including recordings by Dr. Warf himself – more than double what SVP had 18 months ago.
Together, SDSC and NeuroKids are building the future of surgical training: one that doesn’t depend on being in the same operating room, or even the same continent. A future where lifesaving knowledge is scaled, shared, and safeguarded – not hoarded.
“With this work, we are testing a new methodology of training surgeons to learn how to do ETV/CPC, with the intent of increasing the number of capable surgeons, and thus the number of surgeries per year for kids suffering from hydrocephalus, ultimately reducing death from neurologic disease and disability.” – Dr. Daniel Donoho
For more on the lived experience behind this work, you can watch our Data Science Roundtable with Amanda Garzon, COO, and Susan Fiorella, Board member, of the Hydrocephalus Association, who shared how hydrocephalus has touched their own lives.
1. Fallah A, Weil AG, Juraschka K, Ibrahim GM, Wang AC, Crevier L, et al. The importance of extent of choroid plexus cauterization in addition to endoscopic third ventriculostomy for infantile hydrocephalus: A retrospective North American observational study using propensity score–adjusted analysis. Journal of Neurosurgery: Pediatrics. 2017 Dec;20(6):503–10. doi:10.3171/2017.7.peds16379



.png)
.png)